Autistic individuals often navigate healthcare systems that are not designed with their unique sensory, communication, and cognitive needs in mind. As a result, many face challenges not only in accessing appropriate care but also in being understood, believed, and supported by healthcare professionals.
Both medical and mental health providers have the opportunity—and responsibility—to create safer, more accommodating environments that affirm neurodiversity and respect the lived experiences of autistic people. Doing so not only improves health outcomes but also fosters trust and dignity in the therapeutic relationship.
Autism in the Mental Health Setting
Common Barriers in Therapy
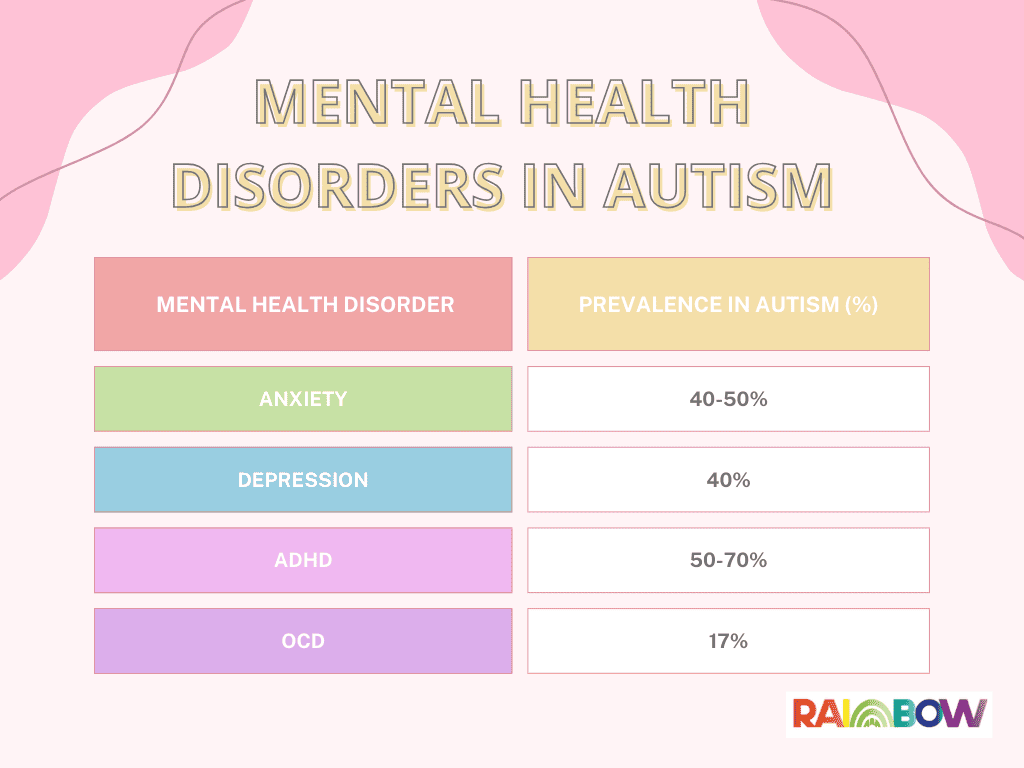
Autistic individuals frequently seek mental health support, often for co-occurring issues like anxiety, depression, trauma, and burnout. Unfortunately, many therapists lack adequate training in recognizing or supporting autism, especially in adults and girls.
Core Needs in Therapy
-
Respect for neurodivergent communication styles
-
Predictability and clear structure in sessions
-
Sensory-safe environments
-
Affirmation of autistic identity without pathologizing
Tips for Mental Health Providers
-
Seek autism-specific training, especially for women and adults.
-
Individualize therapeutic approaches beyond CBT scripts.
-
Offer written materials, visual aids, and routine session outlines.
-
Validate sensory needs and give permission for stimming or comfort items.
-
Encourage self-advocacy and informed consent at every stage.
Autism in the Medical Setting
Challenges
Medical settings can be overwhelming or even traumatic due to:
-
Bright lights, loud noises, and crowded waiting areas
-
Misinterpretation of communication difficulties
-
Dismissal of sensory sensitivities or pain expression
Core Needs in Medical Care
-
Direct, unambiguous language
-
Sensory accommodations (dim lights, quiet spaces)
-
Extra time to process and respond
-
Clear consent practices and gentle physical interaction
Tips for Medical Providers
-
Ask about and note communication/sensory preferences.
-
Narrate procedures and seek verbal or written consent.
-
Avoid rushing appointments—build in quiet processing time.
-
Offer take-home summaries and diagrams or visuals.
-
Be flexible and patient with non-traditional responses or questions.
Your Ally in Autism-Informed Care
Kristen Math, Therapist & Evaluator at Therapy Dynamics
I specialize in comprehensive evaluations for autistic girls and work with families and professionals to create affirming, individualized care plans.
Contact me at kristen@therapydynamics.com for evaluation services, consultation, or autism-informed therapy.
Companion Checklist: Autism-Informed Practices for Providers
Here’s a quick-reference guide for clinicians:
Mental Health Professionals
| Strategy | Action |
|---|---|
| Ask, Don’t Assume | Inquire about sensory needs, communication preferences, and goals. |
| Validate Autistic Identity | Avoid framing autism as a deficit to fix. Emphasize strengths and self-understanding. |
| Predictability Matters | Set session structure, review what to expect. Give prep for changes. |
| Sensory-Friendly Space | Reduce harsh lighting, background noise; allow fidgets or comfort items. |
| Use Visual Aids & Written Summaries | Especially helpful for processing and memory. |
| Avoid Eye Contact Assumptions | Respect varied social cues. Eye contact is not a measure of engagement. |
Medical Professionals (MDs, NPs, PAs)
| Strategy | Action |
|---|---|
| Slow Down | Give time for processing and response. Avoid interrupting silence. |
| Be Direct & Literal | Use concrete, unambiguous language. Avoid euphemisms. |
| Consent is Key | Explain what you’re doing before you do it. Offer choice and control. |
| Prepare for Sensory Triggers | Dim lights, reduce noise, avoid strong smells if possible. |
| Allow Accommodations | Alternative waiting spaces, written communication, or flexible scheduling. |
| Follow Up in Writing | Send clear summaries of procedures, medications, or next steps. |